| Cardiovascular | Lower limb neurology | Peripheral vascular |
| Respiratory | Cranial nerves | Genitourinary |
| Abdominal | Opthalmological | Gynecological |
| Upper limb neurology | Thyroid | Dermatology |
In this section you’ll find comprehensive scripts to guide your examination technique. There also fabulous infographics and videos (created by Nick Smith). The infographics are available as pdfs to download below.
Cardiovascular
Video
Script
Introduction
“Hello, my name is Phil, I am one of the medical students.”
“Please can you confirm your name and date of birth, while I wash my hands, put on my PPE and ensure we are somewhere private.”
“Are you comfortable? Do you need any pain relief or a drink?”
“I have been asked to examine your cardiovascular system. This will involve looking at your hands and face, examining your chest and looking at your legs. Is this ok with you?”
“Would you like a chaperone present?”
“Please can you take your top off?”
“I will ensure the bed is at 45 degrees”
“I will talk out loud as we go”
“If at any time you want me to stop or you are in pain, let me know”
Brief history
“Can you briefly tell me why you have come to hospital?”
General inspection
“I am looking at the…”
Patient’s
- comfort level; respiratory distress
- body habitus
- dysmorphic features
- scars (sternotomy or pacemaker)
Environment
- oxygen
- GTN spray
- walking aids
Hands and other observations
“I am feeling for…”
- warmth
- clamminess
- the pulse (rate; rhythm; quality)
“I am looking for…”
- clubbing
- tar staining
- peripheral cyanosis
- features of endocarditis (e.g. Janeway lesions)
- signs of aortic regurgitation (e.g. head bobbing)
Other observations
- Blood Pressure
- Respiratory Rate
- Oxygen saturations
- Temperature
- Blood glucose
Neck
“I am looking for…”
- Carotid pulse: “I am going to feel the pulses in your neck in turn to assess their quality”
- Jugular venous pressure:
- “I will ensure you are at 45 degrees.
- Please turn your head to the left and relax head on the pillow.
- I am going to press on the upper right side of your abdomen to elicit the hepato-jugular reflex.
- I am measuring the number of centimetres it is from the sternal angle.”
Face
“I am looking for evidence of…”
- Corneal arcus and xanthelasma
- Conjunctival pallor (please look up I will gently lower your bottom eye lids)
- Central cyanosis
- Angular stomatitis of lips
Precordium
Inspection: “I have already commented on.”
“I am palpating…”
- the central capilliary refill time
- the apex beat – 5th intercostal space; midclavicular line
- each valve area for heaves and thrills of palpable murmurs
No percussion
“I am auscultating the…”
- carotids for bruit or radiation of aortic stenosis
- all the heart valves with bell and diaphragm
- for murmurs (including maneuvers to assess for murmurs as indicated by findings)
Additional
“Please can you…”
- lean forward so I can listen to your lungs and press on your lower back to assess for oedema
- lay flat so I can assess for hepatomegaly
- lift your trousers above your knees so I can look for peripheral oedema
Close
“Thank you. That is the end of the examination.”
“Do you need any help getting dressed?”
“In summary my working differential diagnosis is…”
“To complete my examination (scenario dependent) I would like to:
- Examine peripheral pulses: including checking for radio-femoral/radio-radio delay; ankle-brachial pressure index
- Obtain an
- ECG
- chest x-ray,
- lying/standing blood pressure
- urinalysis
- blood tests (state which ones)
“Does that sound reasonable to you? Do you have any questions or concerns?”
Additional Resources
- Cardiovascular exam 1; 2
- Heart murmurs
- JVP assessment
- ECG 1; 2
Respiratory
Video
Script
Introduction
“”Hello, my name is Phil. I am one of the medical students.”
“Please can you confirm your name and date of birth, while I wash my hands, put on my PPE and ensure we are somewhere private.”
“Are you comfortable? Do you need any pain relief or a drink?”
“I have been asked to examine your respiratory system. This will involve looking at your hands and face, examining your chest and looking at your legs. Is this ok with you?”
“Would you like a chaperone present?”
“Please can you take your top off?”
“I will ensure the bed is at 45 degrees”
“I will talk out loud as we go”
“If at any time you want me to stop or you are in pain, let me know”
Brief history
“Can you briefly tell me why you have come to hospital?
General inspection
“I am looking at the…”
Patient’s
- comfort level
- body habitus
- scars from chest drains/aspiration
- chest wall deformity
- respiratory distress and shortness of breath
- cyanosis
Environment
- oxygen
- inhalers/nebulisers
- sputum pots
Hands and other observations
“I am feeling for…”
- warmth
- clamminess
- the pulse (rate; rhythm; quality)
“I am looking for…”
- clubbing
- tar staining
- peripheral cyanosis
- wasting (Pancoast’s tumour)
- CO2 retention tremor
Other observations
- Blood Pressure
- Respiratory Rate
- Oxygen saturations
- Temperature
- Blood glucose
Neck
“I am looking for…”
- Jugular venous pressure:
- “I will ensure you are at 45 degrees.
- Please turn your head to the left and relax head on the pillow.
- I am going to press on the upper right side of your abdomen to elicit the hepato-jugular reflex.
- I am measuring the number of centimetres it is from the sternal angle.”
- Lymph nodes: I need to feel for any glands in your neck. I will stand behind you and feel along your jaw; in front of then behind your ears; down your neck and along your collar bones.
- Trachea position: I need to feel in the space between your collar bones assessing that your windpipe is central.
Face
“I am looking…”
- at your eyes for Horner’s syndrome (ptosis; miosis; ask about anhydrosis)
- for central cyanosis
- for nasal patency (please occlude each nostril in turn and breath in and out. Does it feel equal?)
Chest
“I am looking at the front, sides and then back of the chest…”
Anterior
- inspecting for: scars; bruising and deformity
- palpating for expansion
- percussing
- auscultating for breath sounds and added sounds
- assessing vocal fremitus (say 99 while listening)
Posterior
- inspecting for: scars
- palpating for expansion and oedema
- percussing
- auscultating for breath sounds and added sounds
- assessing vocal fremitus (say 99 while listening)
- Perform either tactile or vocal fremitis. There is no need to do both.
Close
“Thank you. That is the end of the examination.”
“Do you need any help getting dressed?”
“In summary my working differential diagnosis is…”
“To complete my examination (scenario dependent) I would like to:
- Obtain a
- peak flow
- chest x-ray,
- arterial blood gas (if low oxygen saturations)
- sputum sample
- blood tests (state which ones)
“Does that sound reasonable to you? Do you have any questions or concerns?”
Abdominal
Video
Script
Introduction
“”Hello, my name is Phil I am one of the medical students.”
“Please can you confirm your name and date of birth, while I wash my hands, put on my PPE and ensure we are somewhere private.”
“Are you comfortable? Do you need any pain relief or a drink?”
“I have been asked to examine your gastrointestinal system. This will involve looking at your hands and face and chest, then examining your abdomen. Is this ok with you?”
“Would you like a chaperone present?”
“Please can you take your top off?”
“I will ensure the bed is at 45 degrees”
“I will talk out loud as we go”
“If at any time you want me to stop or you are in pain, let me know”
Brief history
“Can you briefly tell me why you have come to hospital?”
General inspection
“I am looking at the…”
Patient’s
- comfort level
- jaundice
- abdominal distension
- abdominal drains or scars
- spider naevi; caput medusa and gynaecomastia
- anasarca
Environment
- drains
Hands and other observations
“I am feeling for…”
- warmth
- clamminess
- the pulse (rate; rhythm; quality)
“I am looking for…”
- clubbing
- leucknoycia
- palmar erythema
- Dupuytren’s contractures
- liver flap
Other observations
- Blood Pressure
- Respiratory Rate
- Oxygen saturations
- Temperature
- Blood glucose
Face
“I am looking for evidence of…”
- conjunctival pallor (“Please look up I will gently lower your bottom eye lids.”)
- cngular stomatitis of lips
- cral ulcers (Please open your mouth and stick out your tongue.”)
- lymph nodes (“I need to feel your neck for any swellings. I will stand behind you to do this.”)
- Virchow’s node can be found in the left supraclavicular fossa and may be a sign of intraabdomminal malignancy
Abdomen
“Now I need to examine your abdomen. Are you ok to lie flat? If at any time you are in pain or want me to stop let me know.”
“I will examine the patient from their right side; at their level; looking at the patient for any signs of discomfort.”
Inspection
- Closer inspection (don’t forget the left flank)
Palpation
- Light then deep all quadrants for: guarding; rigidity; etc
- Organs: liver; spleen; kidney; bladder
- Aorta
Percussion
- Organs: liver; spleen; bladder
- Ascites (shifting dullness)
Auscultation
- Bowel sounds
- Femoral bruits
Close
“Thank you. That is the end of the examination”
“Do you need any help getting dressed?”
“In summary my working differential diagnosis is…”
“To complete my examination (scenario dependent) I would like to:
- Examine the the axilla; groin; the hernial orifices; perform a rectal examination and testicular exam (male patients)
- Obtain a
- urinalysis
- chest x-ray/abdominal x-ray/CT scan
- blood tests (state which ones)
“Does that sound reasonable to you? Do you have any questions or concerns?”
Additional Resources
- Abdominal exam
- PR exam
- Abdominal x-ray: 1 ,2
Upper Limb Neurology
Infographic



Video
Script
Introduction
“Hello, my name is Phil. I am one of the medical students!.
“Please can you confirm your name and date of birth, while I wash my hands, put on my PPE and ensure we are somewhere private.”
“Are you comfortable? Do you need any pain relief or a drink?”
“I have been asked to examine the nerves that supply the upper limbs. This will involve me assessing your strength; sensation; coordination and reflexes in both your arms. Is this ok with you?”
“Would you like a chaperone present?”
“I will ensure the bed is at 45 degrees”
“I will talk out loud as we go”
“If at any time you want me to stop or you are in pain, let me know”
Brief history
“Can you briefly tell me what the problem is?”
“Which hand do you write with?”
“Any trauma?”
“Any hobbies?”
“Are you currently working?”
General inspection
“I am looking at the…”
Patient for (standing; front; back; sides)
- wasting
- fasciculation
- posturing
- scars
Environment
- slings
- splints
Tone
“I am going to hold each of your hands and do some movements with them to assess your tone…” (Flexion; extension; supination and pronation at the elbow)
“I am assessing whether tone is increased, reduced or normal.”
Power
“I need to assess how strong you are by asking you to do some movements…”
Test the different muscle groups
| Shoulder abduction (deltoid) | C5 |
| Elbow extension (triceps) | C7 |
| Elbow flexion (biceps) | C6 |
| Wrist extension (extensor carpi ulnaris+radialis) | C7 |
| Wrist flexion (flexor carpi ulnaris+radialis) | C6 |
| Finger extension | C7 |
| Finger flexion | C8 |
| Finger: abduction; opposition; thumb to ceiling; thumb to middle finger | All T1 |
Sensation
“I need to test how well you can feel areas on your skin…”
- Can you feel here? (on upper chest)
- Bring you arms straight by your side with you palms facing forward (‘anatomical’ position).
- Please can you close your eyes and tell me when you feel something.
“I will assess the different modalities of all dermatomes using:”
- Light touch (cotton wool)
- Sharp/dull (neurotip)
- Vibration sense (128Hz tuning fork): start on a distal bony prominence and move proximally
- Proprioception (joint position sense)
- Temperature
Relexes
“I need to assess your reflexes, I will use the tendon hammer to assess them…”
“Try and relax your arm, I am going to…”
- tap in the crook of your elbow (biceps: C5-6))
- tap on your lower arm just above your wrist on the side where the thumb is (brachioradialis: C6-7)
- to support your arm by interlocking my fingers with yours allowing your elbow to hang down, and tap just above the elbow (triceps: C7-C8)
- You may want to ask the patient to re-enforce the reflexes by clenching their teeth, hooking together their flexed fingers and trying pull them apart.
Coordination
“I need to assess your co-ordination…”
- With your index finger can you touch your nose and then my finger? Keep going back and forth and try to keep following my finger. I will keep my finger still. Please continue with your eyes closed (finger-nose).
- Close your eyes and extend your arms up to the ceiling, palms up and keep them there (pronator drift).
- Can you place your hand into your palm and then move your hand back to front as quickly as you can. Please repeat on the other side (dysdiadochokinesia).
Close
“Thank you. That is the end of the examination”
“Do you need any help getting dressed?”
“In summary I found/did not find…”
“To complete my examination I would like to do a peripheral vascular and neck examination.”(scenario dependent)
“Does that sound reasonable to you? Do you have any questions or concerns?”
Additional Resources
- Upper limb neuro exam
- Upper vs lower motor neurone lesions/signs
- Cerebellar examination (includes upper limb section)
- Ascending and descending tracts
- Dermatomes and myotomes
- Power grading: MRC
- Assessing reflexes
Lower Limb Neurology
Infographic



Video
Script
Introduction
“Hello, my name is Phil. I am one of the medical students.”
“Please can you confirm your name and date of birth, while I wash my hands, put on my PPE and ensure we are somewhere private.”
“Are you comfortable? Do you need any pain relief or a drink?”
“I have been asked to examine the nerves that supply the lower limbs. This will involve me assessing your strength; sensation; coordination and reflexes. Is this ok with you?”
“Would you like a chaperone present?”
“Are you ok to change into shorts?”
“I will talk out loud as we go”
“If at any time you want me to stop or you are in pain, let me know”
Brief history
“Can you briefly tell me what the problem is?”
“Any trauma?”
“Any hobbies?”
“Are you currently working?”
General inspection
“I am looking at the…”
Patient for (standing: front; back; sides)
- gross deformity (varus/valgus)
- wasting
- fasciculations
- I will also assess:
- gait (broad based; shuffling; antalgic)
- hip extension
Environment
- walking aids (crutches; wheelchair; splints)
Tone
“Please sit on the couch with legs out in front of you, I am going to move your legs to look at the tone. I will…”
- roll your legs then ankles (independently) side to side.
- briskly lift your knees up (from underneath) (whole distal leg rises suggests hypertonia).
- briskly lift your ankle up (ankle dorsiflexion) to look for clonus (greater than 5 beats is abnormal).
Power
“I need to assess how strong you are in your legs…”
Test the different muscle groups
| Hip flexion (hold leg up don’t let me push down) | L2/3 |
| Hip extension (push heels into bed) | L4/5 |
| Knee flexion (bend up and pull me into you) | L5/S1 |
| Knee extension (bend up and push me away) | L3/4 |
| Ankle flexion (push ankle down into my hand) | L4/5 |
| Ankle extension (push ankle pull ankle up to ceiling) | S1/2 |
| Inversion (push ankle against hand) | L4 |
| Eversion (push ankle against hand) | L5/S1 |
| Big toe up (push up against finger) | L5 |
| Big toe down (push down against finger) | S1/2 |
Sensation
“I need to test how well you can feel areas on your skin…”
Demonstrate sensation elsewhere first.
Legs in ‘anatomical’ position’
“I will assess the different modalities of all dermatomes using:”
- Light touch (cotton wool)
- Sharp/dull (neurotip)
- Vibration sense (128Hz tuning fork): start on a distal bony prominence and move proximally
- Proprioception (joint position sense)
- Temperature
Relexes
“I need to assess your reflexes, I will use the tendon hammer to assess them…”
“Try and relax your arm, I am going to…”
- tap just below your knee (patella reflex: L3/4).
- to move rotate your foot out and tap the back of your heel (ankle reflex: S1/2).
- tickle the bottom of your feet (plantar response) (Extension = Babinski’s sign = upper motor neurone lesion).
Coordination
“I need to assess your co-ordination…”
- Can you put the heel of one foot below your knee and run your foot up and down your shin with eyes open, and then closed (repeat on other side).
Close
“Thank you. That is the end of the examination”
“Do you need any help getting dressed?”
“In summary I found/did not find…”
“To complete my examination (scenario dependent) I would like to do peripheral vascular, abdominal and hip examination.”
“Does that sound reasonable to you? Do you have any questions or concerns?”
Additional Resources
- Lower limb neurological exam
- Gait abnormalities
- Upper vs lower motor neurone lesions/signs
- Cerebellar examination (includes upper limb section)
- Ascending and descending tracts
- Dermatomes and myotomes
- Power grading: MRC
- Assessing reflexes
Cranial Nerves
Infographic


Video
Script
Introduction
“Hello, my name is Phil. I am one of the medical students”.
“Please can you confirm your name and date of birth, while I wash my hands, put on my PPE and ensure we are somewhere private.”
“Are you comfortable? Do you need any pain relief or a drink?”
“I have been asked to examine your cranial nerves. These are the nerves in your head that supply the face. It will involve me assessing smell, vision, hearing and getting you to do some movements with your face. Is this ok with you?”
“Would you mind sitting in a chair facing me?”
“Would you like a chaperone present?”
“I will talk out loud as we go”
“If at any time you want me to stop or you are in pain, let me know”
Brief history
“Can you briefly tell me why you’ve come to hospital today?”
General inspection
“I am looking at the…”
Patient for
- facial asymmetry
- rashes
- ptosis
- unequal pupils
- scars
” will now examine each nerve in turn…”
Environment
- glasses
- hearing aids
Cranial Nerve Examination
You may want to clarify aspects of the required exmaintion with the examiner. These are hughlighted in blue
Olfactory: Cranial Nerve I
“Have you noticed any change in your sense of smell?”
Examiner: “would you like me to formally examine this?”
Optic: Cranial Nerve II
Visual acuity
- “If you normally wear glasses please put them on, if haven’t got them with you, use pin hole.
- I will use this Snellen chart to assess acuity.
- Please stand here at a distance of six metres from the chart.
- Close one eye, read the lowest line possible, then change side.”
Visual acuity (VA) = 6/number of the line achieved
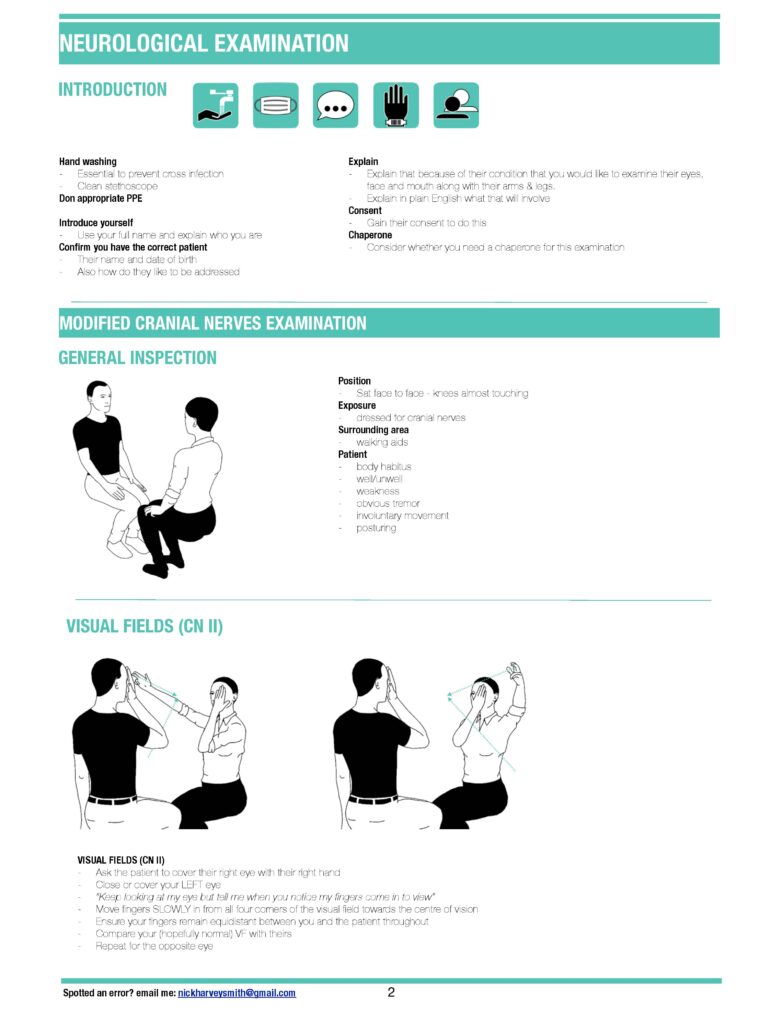
Visual fields
- Please cover one eye. I will cover the opposite and we will look at each in turn
- I will sit opposite you. Please look at my nose; I will bring my finger in from the side, say yes when you see my finger and if you see it disappear at any time (assess 6 quadrants)
Examiner: “Would you like me to formally assess blind spot (red hat pin) or for neglect?”
Colour vision
Examiner: “Would you like me to assess colour vision using Ishihara chart?“
Pupils
“I am looking at the pupils for:
- size
- shape
- regularity
- ptosis
- normal lie
Pupillary reflexes (ask pt to focus on point in distance),
I am assessing for the following pupilliary reflexes:
- Direct
- Consensual
- Swinging-light reflex to assess for a relative afferent pupillary defect
“I would normally now perform…”
- fundoscopy
- slit lamp examination
- eversion of lids if FB concern.
- Examiner: “Would you like me to do this?”
Eye movements: Cranial Nerves III, IV, VI
- “Please keep your head still and follow my finger with you eyes.
- Tell if you have any pain or double or blurred vision.
- I am looking for nystagmus and ptosis.”
Trigeminal: Cranial Nerve V
Motor
“Please can you clench and relax your teeth?”
“I am feeling over the:”
- Masster
- Temporalis
Sensory
“Can you feel me touch you (dull, sharp, light etc)”…
- ophthalmic
- maxillary
- mandibular divisions?
“Does it feel the same on both sides?”
Reflexes
Examiner: “would you like me to assess…”
- Corneal reflex
- Jaw jerk
Facial: Cranial Nerve VII
Motor (muscles of facial expression)
- “Show me teeth; puff your cheeks out; purse your lips.
- Close your eyes tight; don’t let me open them.
- Open your eyes wide; don’t let me close them
Sensory
Altered:
- hearing (hyperacusis)
- taste
Vestibocochlear: Cranial Nerve VIII
Vestibular
“I will examine each ear in turn…”
Otoscopy
- Examiner: “I would normally perform otoscopy as part of my assessment. Would you like me to do this?”
Whisper test
- “I am going to rub my fingers in front of one ear and whisper a number in the other.
- What is the number I whispered?”
Rinne Test
- “I am going to tap the tuning fork and place it behind your ear and then in front.
- Do you hear it louder behind or in front of the ear?”
Weber Test
- “I am going to tap the tuning for and place it on the top of your head.
- Do you hear it equally in both ears, or is one side louder?”
Cochlear
- Scenario dependent, to the examiner: “This sounds like….. Would you like me to assess using:”
- Dix-Hallpike for ?benign paroxysmal positional vertigo
- HINTS if persistent/continuous vertigo and nystagmus and considering central vs peripheral cause
- Turning test
Glossopharyngeal: Cranial Nerve IX
Motor
Examiner: “Would you like me to test the gag reflex (afferent part)?”
Sensory
Altered taste
Vagus: Cranial Nerve X
Motor
- “Open your mouth and say ‘ahhh’” (assessing uvula position and palate symmetry)
- Examiner: “Would you like me to test the gag reflex (efferent part)?”
Accessory: Cranial Nerve XI
Motor
- “Can you shrug your shoulders?” (assessing trapezius strength)
- “Turn your head into my hand?” (assessing sternocleidomastoid on both sides)
Hypoglossal: Cranial Nerve XII
Motor
- “Can you stick out your tongue?” (assessing for fasiculation and wasting)
- “Can you push your tongue into your cheek and don’t let me push it in.” (assess each side)
Close
“Thank you. That is the end of the examination”
“In summary I found/did not find…”
“To complete my examination (scenario dependent) I would like to…”
“Does that sound reasonable to you? Do you have any questions or concerns?”
Opthalmological
Introduction
“Hello, my name is Phil. I am one of the medical students”.
“Please can you confirm your name and date of birth, while I wash my hands, put on my PPE and ensure we are somewhere private.”
“Are you comfortable? Do you need any pain relief or a drink?”
“I have been asked to examine your eyes. This will involve me looking at them directly and with a light source; testing your vision; eye movements, and reflexes. Is that ok with you?”
“Would you like a chaperone present?”
“I will talk out loud as we go”
“If at any time you want me to stop or you are in pain, let me know”
Brief history
“Can you briefly tell me what the problem is?
“Any trauma or injury?”
“Do you wear glasses or contact lenses normally? Have you got them with you?”
General inspection
Face the patient
“In terms of general inspection I am looking at the…”
- External eye appearances: ptosis; proptosis; squint; head tilt; pupil symmetry
- Lids; lashes; lacrimal gland and duct: swelling of lids; position (ectropion/entropion); blepharitis; blepharospasm; follicles; crusting/pus
- Cornea; conjunctiva; sclera: Cornea (white/hazy); sclera (injection – diffuse/local)
- Foreign bodies: Examiner: “would you like me to evert eyelids, fluorescein and assess using the slit lamp?”
Pupils
- Appearance: size; shape; symmetry
- Reflexes
- Direct
- Consensual
- Swinging light test (RAPD – Marcus Gunn pupil)
- Accommodation: please focus on something in the background; now looking at my finger (pupils constrict on focusing from far to near objects)
- Squint: cover/uncover test
Visual acuity
“If you normally wear glasses please put them on. If haven’t got them with you I will use a pin hole.” (If vision improves this suggests a refractive error)
“I will examine each eye in turn…”
Far vision
- “I will use this Snellen chart to assess acuity
- Please stand here at a distance of six metres from the chart
- Close one eye, read lowest line possible, then change side
Visual acuity(V/A) = 6/number of line achieved
Near vision
Examiner: would you like me to assess near vision by asking the patient to read a sentence from a book?
Colour vision
Examiner: would you like me to assess colour vision using the Ishihara plates?
Visual fields
“Please cover one eye. I will cover the opposite and we will look at each in turn…”
“I will sit opposite you. Please look at my nose, I will bring my finger in from the side, say yes when you see my finger and if you see it disappear at any time (assess 6 quadrants)…”
Examiner: “would you like me to formally assess blind spot (red hat pin) or for neglect?”
Eye movements
“Follow my finger with your eyes keeping your head still. Tell me if you get any pain or double vision.”
Examiner: “I am looking for nystagmus and ptosis.”
Fundoscopy
“I would do this in a dark room, having dilated the pupils with a short acting drop like 1% tropicamide. I will have informed the patient that they cannot drive until their vision is back to normal.”
I am examining the:
- Red reflex
- Retina (start lateral, find a vessel and move in), paying particular attention to:
- Optic disc (normal cup/disc ratio 0.3)
- Retinal vessels (tortuous; nipping; neovascularisation; haemorrhage)
- Macula (“Please look into my light” -cherry red = CRAO, drusen = mac degen
Close
“Thank you. That is the end of the examination”
“To complete my examination I would like to…”
- perform a slit lamp exam,
- check intraoccular pressures,
- a full cranial nerve examination,
- assess for risk factors for GCA and investigate as needed
“Does that sound reasonable to you? Do you have any questions or concerns?
Additional resources
- Examination of the eyes and vision
- Fundoscopy
- NICE: Eye conditions overview
- Geeky medics (eyelid disorders; red eye: painless and painful; acute angle closure glaucoma; retinal detachment; painless sudden visual loss; orbital and periorbital cellulitis; eye drops
- Also see cranial nerve additional resources above
Thyroid
Introduction
“Hello, my name is Phil. I am one of the medical students”.
“Please can you confirm your name and date of birth, while I wash my hands, put on my PPE and ensure we are somewhere private.”
“Are you comfortable? Do you need any pain relief or a drink?”
“I have been asked to examine you to assess whether your thyroid maybe causing any of your symptoms. This will involve me: examining your hands; face; neck; legs and reflexes. Is this ok with you?”
“I will talk out loud as we go”
“If at any time you want me to stop or you are in pain, let me know”
Brief history
“Can you briefly tell me why you have come to hospital?”
General inspection
“I am looking at the patient for signs of…”
- Flushing
- Loss of outer ⅓ eyebrow
- Tremor
- Obvious eye signs
- Neck swelling or scars around the neck
- Body habitus
Hands and other observations
“I am feeling for…”
- warmth
- clamminess
- the pulse (rate; rhythm; quality)
“I am looking for…”
- Tremor (hold hands out)
- Nail changes (onycholysis; thyroid acropachy)
- Palmar erythema
- Thick coarse skin
Other observations
- BP
- Resp Rate
- Sats
- Temperature
- Blood glucose
Face
“I am looking for…”
- Eyebrow: loss of outer ⅓
- Eye signs:
- lid retraction
- Lid lag on downwards gaze (“Please look down for me“)
- Proptosis (“I will assess by looking from the side and down”)
- Eye movements: “Please follow my finger with your eyes and tell me if you get any double vision.”
Neck
Inspection
“I am looking at the neck from the front and side for masses/swellings or scars”
Palpation
“I need to feel your neck:“
- Trachea central?
- Masses: size; shape; nodule; diffuse
- “Please can you take a sip of water and swallow” (thyroid masses rises on swallow)
- “Please can you stick out you tongue” (thyroglossal cysts will move on sticking the tongue out)
- I am just going to feel for any other lumps in the neck (Lymph nodes)
Percussion
“I am going to tap along your breast bone (dull on percussion suggests a retrosternal goitre)
Auscultation
“I am just going to listen to the neck” (assessing for bruits)
Lower limb reflexes
“Lastly I would like to…”
- Look at your shins for any evidence of pretibial myxoedema
- Test your reflexes
Close
“Thank you. That is the end of the examination”
“In summary my working differential diagnosis is…”
“To complete my examination I would like to do the following investigations/tests…”
“Does that sound reasonable to you? Do you have any questions or concerns?”
Additional resources
- Thyroid exam 1, 2
- Neck lumps 1, 2, 3
- Hyperthyroidism and thyrotoxicosis 1, 2
- Hypothyroidism
- Thyroid function tests
Peripheral vascular
Introduction
“Hello, my name is Phil. I am one of the medical students.”
“Please can you confirm your name and date of birth, while I wash my hands, put on my PPE and ensure we are somewhere private.”
“Are you comfortable? Do you need any pain relief or a drink?”
I have been asked to conduct an examination of your peripheral vascular system. This means assessing the blood supply to your limbs; doing some tests to assess the supply; feeling your pulses and also an abdominal examination. You will need to have your legs exposed up to your groin. Would this be ok with you?
“I will talk out loud as we go”
“If at any time you want me to stop or you are in pain, let me know”
Brief history
“Can you briefly tell me why you have come to hospital?
General inspection
“I am looking at the patient for signs of…”
- habitus (obese or cachetic)
- scars
- distended abdomen
- expansile abdominal mass
Legs
Inspection
- skin colour
- chronic changes e.g. hair loss; ulcers
- oedema: unilateral; bilateral; extent
- scars
- varicose or dilated veins
- infection
- gangrene
- Toes: web spaces and heels
Palpation
- Temperature (dorsum hand long leg)
- Tenderness
- Capillary refill
- Pulses: dorsalis pedis; posterior tibial; popliteal; femoral – compare left to right
- Oedema: pitting vs non pitting
- Circumference
- Sensation; reduced or hyperaesthesia
Move
“Can you wiggle your toes for me?”
Special tests
- Doppler ultrasound (if difficulty feeling pulses at feet)
- Buerger’s test
- Ankle brachial pressure index
Buerger’s test
Two stages:
- ELEVATION = pallor
- Raise legs 45o 2-3 minutes; look for pallor on the sole of foot (if develops, note angle)
- Normal = stay pink with elevation at 90o
2. DEPRESSION = hyperaemia
- Sit patient up; hand legs over side of bed
- Note colour change of the foot
- Normal = rapidly pink
- Limb ischaemia = slow return, bright red
Ankle-brachial pressure index
- Highest SBP in arms.
- BP cuff around leg; inflate cuff to above systolic (use doppler); then deflate cuff and measure when flow returns
- Do for Dorsalis pedis and posterior tibial
- Divide ankle by arm to obtain value.
- Normal = 1.0-1.2.
- Mild disease = 0.5-0.8
- Severe disease = <0.5
Close
“Thank you. That is the end of the examination”
“To complete my examination I would like to do a…”
- CVS examination (including listening for carotid bruits)
- Abdominal exam (including listening for femoral bruits)
- Abdominal US
“In summary my working differential diagnosis is…”
“To complete my examination I would like to do the following investigations/tests…”
“Does that sound reasonable to you? Do you have any questions or concerns?”
Additional resources
Genitourinary
Introduction
“Hello, my name is Dr Smith I am one of the Senior Doctors working in the Emergency Department today.”
“Please can you confirm your name and date of birth, while I wash my hands, put on my PPE and ensure we are somewhere private.”
“Are you comfortable? Do you need any pain relief or a drink?”
“I have been asked to conduct an examination of your genitourinary system. This will involve me examining your abdomen; groin; scrotum and penis”
“We will have a chaperone present?”
“I will talk out loud as we go”
“If at any time you want me to stop or you are in pain, let me know”
“I will close the curtains to ensure privacy and wait outside to allow you to undress from the waist. There is a blanket you can use to cover yourself.“
Brief history
“Can you briefly tell me why you have come to hospital?”
General inspection
“I am looking at the patient for signs of…”
- pain
- gait (if seen walking)
Abdominal examination
“Now I need to examine your abdomen. Are you ok to lie flat? If at any time you are in pain or want me to stop let me know…”
At patients level, keep looking at the patient
Inspection
- Closer inspection, particularly left flank
Palpation
- Light then deep all quadrants for: guarding; rigidity; etc
- Organs: liver; spleen; kidney; bladder
- Aorta
Percussion
- Organs: liver; spleen; bladder
- Ascites (shifting dullness)
Auscultation
- Bowel sounds
- Femoral bruits
Testicular/penile examination
“I now need to examine your testicles and penis. Are you happy for me to continue?..”
Testes/scrotum
Inspection
- colour
- swelling
- transillumination
Palpation
- size; shape; consistency; mass
- epididymis
- lift scrotum (Phren’s sign)
- cremasteric reflex
Penis
- erythema
- vesicles
- ulcers
- discharge (if present -swab; urine dip and send for microscop, culture and sensitivity)
Close
“Thank you. That is the end of the examination”
“In summary my working differential diagnosis is…”
“To complete my examination I would like to do the following investigations/tests…”
“Does that sound reasonable to you? Do you have any questions or concerns?”
Additional resources
- Scrotal pain and swelling
- Testicular examination
- Penile swelling 1, 2
- UTI: men
- Urinalysis
Gynaecological
Introduction
“Hello, my name is Phil. I am one of the medical students.”
“Please can you confirm your name and date of birth, while I wash my hands, put on my PPE and ensure we are somewhere private.”
“Are you comfortable? Do you need any pain relief or a drink?”
“Would you like a chaperone present?”
“I will talk out loud as we go”
“If at any time you want me to stop or you are in pain, let me know”
“I will close the curtains to ensure privacy and wait outside to allow you to undress from the waist. There is a blanket you can use to cover yourself.“
Brief history
Will be scenario dependant. Often the examination is required to remove a retained foreign body (tampn or condom).
“Can you briefly tell me why you have come to hospital?”
“Based on what you have told me you are concerned about retained tampon/condom. Is that correct?”
“Can you tell about: when this happened; and brief gynae history (focus on symptoms; sexual activity; current contraception).”
Plan
Will be scenario dependant.
“I think what we need to do is try to remove…”
“This will involve me examining your abdomen for any pain and then an internal examination, which will involve my firstly the placing two fingers in your vagina and pressing on your abdomen to assess whether there is any tenderness, followed by the use a speculum to help visualise and remove…”
“Have you understood what I have said, or is there anything you want to clarify or go over again?”
“I will ensure you are in a private room and a female chaperone will be present.”
“If at any time you want to stop or you are in pain please let me know.”
“Do you wish to continue with the examination?”
Preparation/Procedure
“Now I need to examine your abdomen. Are you ok to lie flat? If at any time you are in pain or want me to stop let me know…”
Patient
“While I go and get my equipment:
- “Please can you remove the bottom half of your clothes.
- “Sit on the couch and cover yourself with the blanket.”
Equipment
- Speculum (warmed with running water and lubricated with KY-jelly)
- Good light source
- Gloves
- Magill forceps
Wash hands and put on gloves and apron
Patient position
- “Please could you
- lie flat on the bed
- bring yourself around halfway down the bed
- place your hands under your lower back
- bring your ankles together close to your bottom and
- then let you knees fall to the side”
- Optimise light source
Inspection
“I am inspecting the…”
- Perineum for: warts; ulcers; signs of inflammation; discharge
- Inspect clitorus and urethral meatus
- “Please can you cough: looking for stress incontinence; prolapse
Vaginal exam:
Lubricates fingers
“I am just going to insert my fingers into your vagina. Try and concentrate on your breathing, but do let me know if you want me to stop.”
Insert fingers: “I am going to gently pressure on your lower abdomen.”
I am assessing:
- vaginal walls
- cervix and os
- uterus: masses; shape; position
- adenexae to the left and right
“Was there anything particularly tender?”
“Are you ok for me to continue?”
Speculum exam:
- “I am going to do the speculum exam and attempt to visualise and remove…”
- “I am just going to warm the speculum and apply some lubricant.”
- “Take a breath in and try to relax as best you can.”
- Separate labia with on hand and insert at the 3’o’clock position, then rotate to 12’o’clock and gentle open.
- Once cervix/foreign body is in view, I will tighten the screw to maintain position
- “I am using my Magill forceps to remove the foreign body.”
- “I will inspect to ensure all is removed.”
- “I will then loosen the speculum and remove.”
“Well done, it has been removed. Are you ok?”
“I will give you some privacy to get changed and then there are a couple of things we need to discuss.”
Discussion
Will depend on the scenario:
- Retained condom: discussion around: STI screens; emergency contraception.
- Retained tampon: requires safety netting around toxic shock syndrome.
- Retained clot/products in suspected miscarriage:
- Fit for discharge: arranging early pregnancy unit follow up and safety net.
- Needs admission/further treatment: manage haemorrhage and urgent referral.
Close
“Do you have any further questions or concerns?”
Additional resources
- PV exam
- Speculum exam
- Taking swabs
- Contraception: 1, 2
Dermatology
Introduction
“Hello, my name is Phil. I am one of the medical students”
“Please can you confirm your name and date of birth, while I wash my hands, put on my PPE and ensure we are somewhere private.”
“Are you comfortable? Do you need any pain relief or a drink?”
“I have been asked to see you because of a rash, is that correct? I will need to examine this rash, and also look at your mouth, scalp and eyes.”
“Would you like a chaperone present?”
“I will talk out loud as we go”
“If at any time you want me to stop or you are in pain, let me know”
Brief history
“Briefly tell me about this rash.”
- Recent medications
- Change in cosmetics/cleaning products
- Illnesses
- Foreign travel
- Systemic symptoms
General inspection
“In terms of general inspection I am assessing…”
Patient’s appearance
- level of comfort
- location of rash: symmetrical or extremities
Observations
- BP
- Resp Rate
- Sats
- Temperature
- Blood glucose
Closer inspection
“I will need to examine your rash…”
- Describe characteristics of rash using SOCRATES (see Chapter 3)
- Examines: hair; eyes; mouth; lymph nodes
- If appropriate comment on the need to examine the genitalia
Close
“Thank you very much the examination is now over.”
“Would you like any help getting changed?”
“In summary my working differential diagnosis is…
“I think we should try, e.g.
- Dry: emollient: weak steroids
- Itchy: antihistamines
- Infected: topical fusidic acid; flucloxacillin
“Does that sound reasonable to you? Do you have any questions or concerns?”




















