Pick ‘n’ Mix Week 3 February 2023
We are really grateful to Trudie Pestell for sharing this fabulous education initiative that she has been producing for University Hospital Southampton Emergency Department for a while.
Each week we will bring you some clinical pearls to add in to your knowledge and understanding with links to other resources as well as an OSCE of the week.
OSCE of the Week – Cranial Nerves
Use this to practise your abdominal examination. Remember there are resources for lots more system examinations here.
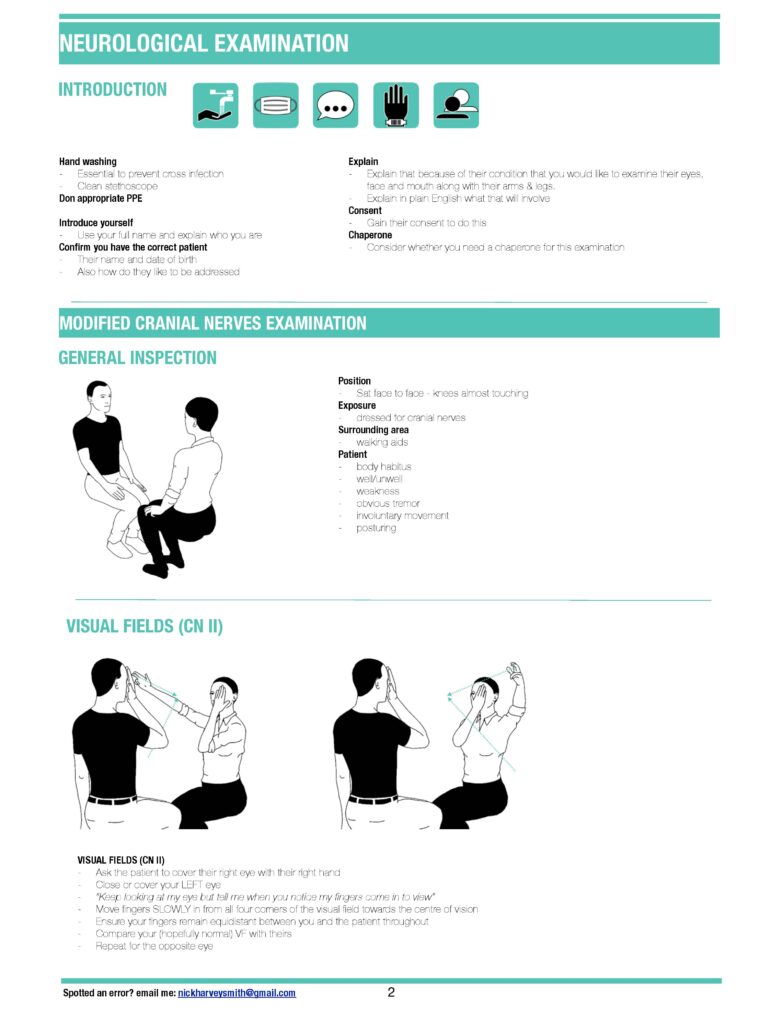
Infographic


Video
Script
Introduction
“Hello, my name is Phil. I am one of the medical students”.
“Please can you confirm your name and date of birth, while I wash my hands, put on my PPE and ensure we are somewhere private.”
“Are you comfortable? Do you need any pain relief or a drink?”
“I have been asked to examine your cranial nerves. These are the nerves in your head that supply the face. It will involve me assessing smell, vision, hearing and getting you to do some movements with your face. Is this ok with you?”
“Would you mind sitting in a chair facing me?”
“Would you like a chaperone present?”
“I will talk out loud as we go”
“If at any time you want me to stop or you are in pain, let me know”
Brief history
“Can you briefly tell me why you’ve come to hospital today?”
General inspection
“I am looking at the…”
Patient for
- facial asymmetry
- rashes
- ptosis
- unequal pupils
- scars
” will now examine each nerve in turn…”
Environment
- glasses
- hearing aids
Cranial Nerve Examination
You may want to clarify aspects of the required exmaintion with the examiner. These are hughlighted in blue
Olfactory: Cranial Nerve I
“Have you noticed any change in your sense of smell?”
Examiner: “would you like me to formally examine this?”
Optic: Cranial Nerve II
Visual acuity
- “If you normally wear glasses please put them on, if haven’t got them with you, use pin hole.
- I will use this Snellen chart to assess acuity.
- Please stand here at a distance of six metres from the chart.
- Close one eye, read the lowest line possible, then change side.”
Visual acuity (VA) = 6/number of the line achieved
Visual fields
- Please cover one eye. I will cover the opposite and we will look at each in turn
- I will sit opposite you. Please look at my nose; I will bring my finger in from the side, say yes when you see my finger and if you see it disappear at any time (assess 6 quadrants)
Examiner: “Would you like me to formally assess blind spot (red hat pin) or for neglect?”
Colour vision
Examiner: “Would you like me to assess colour vision using Ishihara chart?“
Pupils
“I am looking at the pupils for:
- size
- shape
- regularity
- ptosis
- normal lie
Pupillary reflexes (ask pt to focus on point in distance),
I am assessing for the following pupilliary reflexes:
- Direct
- Consensual
- Swinging-light reflex to assess for a relative afferent pupillary defect
“I would normally now perform…”
- fundoscopy
- slit lamp examination
- eversion of lids if FB concern.
- Examiner: “Would you like me to do this?”
Eye movements: Cranial Nerves III, IV, VI
- “Please keep your head still and follow my finger with you eyes.
- Tell if you have any pain or double or blurred vision.
- I am looking for nystagmus and ptosis.”
Trigeminal: Cranial Nerve V
Motor
“Please can you clench and relax your teeth?”
“I am feeling over the:”
- Masster
- Temporalis
Sensory
“Can you feel me touch you (dull, sharp, light etc)”…
- ophthalmic
- maxillary
- mandibular divisions?
“Does it feel the same on both sides?”
Reflexes
Examiner: “would you like me to assess…”
- Corneal reflex
- Jaw jerk
Facial: Cranial Nerve VII
Motor (muscles of facial expression)
- “Show me teeth; puff your cheeks out; purse your lips.
- Close your eyes tight; don’t let me open them.
- Open your eyes wide; don’t let me close them
Sensory
Altered:
- hearing (hyperacusis)
- taste
Vestibocochlear: Cranial Nerve VIII
Vestibular
“I will examine each ear in turn…”
Otoscopy
- Examiner: “I would normally perform otoscopy as part of my assessment. Would you like me to do this?”
Whisper test
- “I am going to rub my fingers in front of one ear and whisper a number in the other.
- What is the number I whispered?”
Rinne Test
- “I am going to tap the tuning fork and place it behind your ear and then in front.
- Do you hear it louder behind or in front of the ear?”
Weber Test
- “I am going to tap the tuning for and place it on the top of your head.
- Do you hear it equally in both ears, or is one side louder?”
Cochlear
- Scenario dependent, to the examiner: “This sounds like….. Would you like me to assess using:”
- Dix-Hallpike for ?benign paroxysmal positional vertigo
- HINTS if persistent/continuous vertigo and nystagmus and considering central vs peripheral cause
- Turning test
Glossopharyngeal: Cranial Nerve IX
Motor
Examiner: “Would you like me to test the gag reflex (afferent part)?”
Sensory
Altered taste
Vagus: Cranial Nerve X
Motor
- “Open your mouth and say ‘ahhh’” (assessing uvula position and palate symmetry)
- Examiner: “Would you like me to test the gag reflex (efferent part)?”
Accessory: Cranial Nerve XI
Motor
- “Can you shrug your shoulders?” (assessing trapezius strength)
- “Turn your head into my hand?” (assessing sternocleidomastoid on both sides)
Hypoglossal: Cranial Nerve XII
Motor
- “Can you stick out your tongue?” (assessing for fasiculation and wasting)
- “Can you push your tongue into your cheek and don’t let me push it in.” (assess each side)
Close
“Thank you. That is the end of the examination”
“In summary I found/did not find…”
“To complete my examination (scenario dependent) I would like to…”
“Does that sound reasonable to you? Do you have any questions or concerns?”


